The Current Evidence for Static Progressive Orthoses for the Upper Extremity
Article by Debby Schwartz published in the ASHT Times Jan 2016
Download the entire study (PDF) here >>
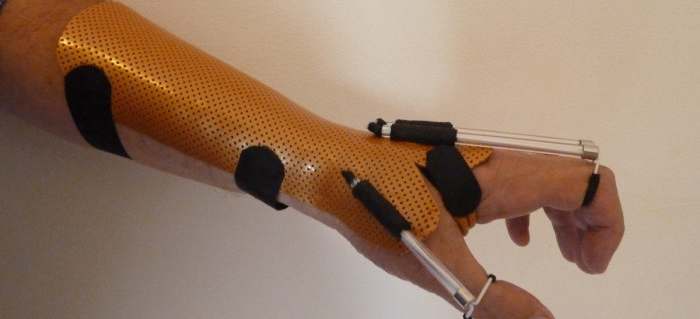
Static progressive orthoses is a type of mobilization orthosis that therapists use to help their clients regain passive motion in stiff joints and tissues.This type of orthosis incorporates non-elastic components to apply force to the stiff joint or tissue, holding it at end-range position to improve passive motion. The client is instructed to increase the force as the joint or tissue accommodates a new end-range position over time. In this manner, static progressive orthoses permits progressive changes in tissue position.

Reaching Plastic Deformation of Tissue
According to Ulrich et al (references via the download below) connective tissue is capable of being stretched due to its viscoelastic qualities. While under tension, it can respond by reaching an either elastic or plastic deformation state. Elastic deformation means that the tissue reverts back to its original length when the force on it is removed and this is undesirable. Plastic deformation means the tissue will maintain its new length even when the force is removed, leading to a structural change in the tissue itself.
Dynamic and static progressive orthoses have been used to apply force to tight or shortened tissue to accelerate tissue remodeling. There are two types of loading conditions with the application of mobilizing orthoses, creep based and stress relaxation. In creep-based loading, the force applied is a constant force and the displacement of the limb varies. Creep-based loading is delivered via dynamic orthoses. However, there are disadvantages to creep-based loading. These orthoses may need to be worn for 6–12 hours daily, treatment may be painful and the joint may be damaged by prolonged compression.
In stress relaxation, the displacement is constant and the applied force varies. This is the principle of static progressive orthoses, in which patients are instructed to constantly adjust and readjust the tension on their stiff joints. The tissue reaches the plastic deformation state more quickly and the effects will last longer.
Static Progressive Orthoses
There are a limited number of studies on the use of static progressive orthoses with a small number of clients enrolled. This review examines the current levels of evidence supporting the use of static progressive orthoses for clients with limitations in range of motion (ROM) of the upper extremity following surgery or trauma (orthopedic pathologies). It also offers relevant information on the types of diagnoses to be treated, wearing schedules, the outcomes affected and the recommended duration of orthotic use.
Key Features
- Non-elastic component places tension on stiff joint/tissue to hold at its maximum tolerable length.
- Adjustments to the tension on each joint can be made by the client.
- The orthotic design maintains the shortened tissue at its maximal tolerable length and does not stress beyond it. It is very important not to exceed the maximal tolerable stress level, which could lead to tissue failure.
- The longer the tissues remains at its maximum tolerable length, the more it increases in length. This concept is known as total end range time (TERT).
- Success can be measured by small gains of perhaps 5–10 degrees a week.
The Benefits
- Improved range of motion without pain; high tolerance for orthotic use because the patient can control the force of the tension; higher compliance and higher patient satisfaction result.
- The patient is able to adjust the tension force gradually, as this type of orthotic intervention takes advantage of small incremental changes in tissue length.
- The optimum orthotic design allows for small changes in joint motion without remolding of the orthosis each time gains in range of motion are accomplished.
Read the entire study (PDF) here >>
![]()

Written by Debby Schwartz, OTD, OTR/L, CHT
Physical Rehabilitation Product and Educational Specialist at Orfit Industries America.
Debby is a certified hand therapist with over 36 years of clinical experience. She completed her Doctorate of Occupational Therapy at Rocky Mountain University of Health Professions in 2010. She has worked at Orfit Industries America as Product and Educational Specialist since 2007.
Debby is also an adjunct professor at the Occupational Therapy Department of Touro University, School of Health Sciences, and at the Occupational Therapy Department at Yeshiva University, Katz School of Science and Health in NYC. She has written many book chapters in the field of hand therapy and multiple articles for hand therapy journals, including the ASHT Times and the Journal of Hand Therapy. She has published a new textbook on orthotic fabrication together with Dr. Katherine Schofield, entitled “Orthotic Design and Fabrication for the Upper Extremity: A Practical Guide”.
![]()
Contact us for more product information or find your local distributor here.
![]()
If you’d like to receive the latest product updates and interesting Orfit news, subscribe to our newsletter: